Episode Transcript
Transcripts are displayed as originally observed. Some content, including advertisements may have changed.
Use Ctrl + F to search
50:00
Methadone Clinic. And if you don't, well, that's a
50:02
different, that's a different episode that we're going to
50:04
do in the future. And I'm just putting it
50:06
out there on how to make new Methadone Clinics
50:08
happen. But you need to know who those
50:10
people are, which means you need to pick up the phone and
50:13
call and say, Hey, I'm a primary care doctor. I'm the medical
50:15
director of a local primary care site. And we want to meet
50:17
you. We want to know your policies and procedures. We want to
50:19
know your walk-in days. We want to know your take-home bottles. We
50:21
want to understand Methadone. Will you come give us a talk? Can
50:23
I pick up the phone at any point and talk to you?
50:26
We do that in primary care with all the
50:28
other specialties. You know, I have everybody's text number
50:30
on my cell phone, right? The GI doctor, the
50:33
OB, the nurse midwife, I have them all. And
50:35
I call them all the time when I have
50:37
a question. We should be able to
50:39
do that with our local OTP. It's critically important,
50:41
partly to get your patients in there, partly to
50:44
advocate for them. Because in a case that David's
50:46
describing, a primary care doctor calling and saying, look,
50:48
do you know how well this person is doing?
50:50
And I heard their bottles are being taken away.
50:52
And I just want to understand that more. I
50:54
wanted to understand what it is you're thinking, what
50:57
can I do to document or help support this
50:59
patient during this time as well, so that we
51:01
don't lose them to treatment and have them have
51:03
the risk of dying? We know that being on
51:05
80 or 100 milligrams of
51:08
Methadone is this threshold to really
51:10
prevent overdose death. And the
51:12
most important thing is that people have Methadone in their
51:14
bodies every single day. I don't care how it happens.
51:16
That's the most important thing. The other thing I'm going
51:18
to say to you is that in the final rule,
51:21
it allows primary care to do the screening
51:23
to say that David has an opiate use
51:26
disorder. I'm really worried about him. He's been
51:28
on Bup with me. It isn't working. He's
51:30
really struggling. I'm going to send
51:32
you my most recent physical. It does not have to
51:34
be a complicated physical. It just has to document some
51:36
vital signs and a couple of physical exam findings. And
51:40
your documentation as a primary care doctor
51:42
that this person has moderate to severe
51:44
opiate use disorder based on your evaluation
51:46
as a licensed clinician. Maybe there's
51:48
a drug screen there. Maybe there's a historical
51:51
drug screen if you want to send that. If you
51:53
have recent labs that will prevent David from having to
51:55
do the labs again, and you
51:57
can send it to the OTP, and that
51:59
is the entry point for them to start
52:01
on methadone. Now, it is the
52:04
licensed clinicians on site that determine the dose.
52:06
They screen, they read what you sent them,
52:08
and they say, wow, David really has opiate
52:10
use disorder. He needs care. I'm going to
52:12
make a decision based on the referral that
52:14
came from Carolyn on how I'm going to
52:17
dose him tomorrow and we'll check in with
52:19
him. The OTP system has to
52:21
do the physical within 14 days after that,
52:23
but it's a low barrier entry. Every primary
52:25
care doctor out there needs to know about
52:28
this because you may know it, ahead of
52:30
your local OTP. We'll
52:32
have things in the show notes that
52:34
help advocate for this process. Yeah.
52:37
I feel like it's really good to hear, even
52:40
though we silo methadone and treatment, it
52:42
is medical care and we should be integrating it
52:44
into our primary care as much as possible, instead
52:47
of just throwing it on a problem list and
52:49
never talking about it. I
52:52
think it's great to hear that, and I think this is
52:54
some news to me too about the final rule and how
52:56
much more of a role we
52:58
can play in lowering barriers to get into
53:00
the OTP, as long as we get to
53:02
know our local resources too. I'll say there
53:04
are other things that you can talk to
53:06
your OTP about too, to lower barriers like
53:08
I know one of the local OTPs we
53:10
work with, instead of taking government IDs, we'll
53:12
take medical records like with a picture and
53:14
their name and address as an alternative to
53:16
the government ID and a lot of Medicaid's
53:18
that offer transportation benefits. There's a lot of
53:20
things you can do to facilitate entry into
53:23
this methadone system and helping people continue on it
53:26
too. Totally. I think exactly
53:28
like you said, Ruth, you won't know how
53:30
you can help until you talk to your
53:32
local OTP, because there is a ton of
53:34
variability. I do want to touch
53:36
upon another challenge that we
53:38
face for patients who are on methadone,
53:41
or who maybe start methadone in the
53:43
hospital, who need to go to a
53:45
skilled nursing facility, maybe for prolonged antibiotics
53:48
or just for rehab, because they
53:50
had some injury where they would
53:52
benefit for more intensive physical therapy
53:54
because we see this issue all
53:56
the time where we hear that
53:59
short term. facilities won't take patients
54:01
on methadone. And
54:03
I'm curious, Ruth, from your
54:06
point of view, how do we sort of
54:08
troubleshoot this in terms of
54:10
helping patients access methadone and
54:12
skilled nursing facilities? Well,
54:15
I'm gonna say the first strong statement, which is it
54:17
is against the federal law to
54:20
deny access to methadone or buprenorphine at a skilled
54:22
nursing facility. So it is a violation of the
54:24
Americans with Disability Act and the Department of Justice
54:26
will come after you. So that's the first thing.
54:28
And it depends on who your Department of Justice
54:30
is, how aggressive they'll be. I'm in a part
54:32
of the country where my assistant
54:34
attorney goes after every single skilled nursing facility. And
54:36
yet we know that skilled nursing facilities will say,
54:38
oh, we didn't not take them because of the
54:40
methadone. We didn't take them for 12 other
54:43
reasons, most of which seemed bogus. So
54:45
that's the first thing. It's against the law, period.
54:48
And a lot of us work in nursing homes. I
54:50
mean, I worked in nursing homes forever as a primary
54:52
care doctor, and it was part of my gig. And
54:54
so if you're one of those primary care people out
54:56
there who also sees people at a skilled nursing facility,
54:59
you should be working from within to make
55:01
sure that that's changed. It's really just stigma.
55:04
It's that people don't want that type of
55:06
person in their facility. Well, you have all
55:08
people in your facility. And
55:10
how to advocate. So then
55:12
that's why you're best friends with your
55:14
OTP medical director, because you can do
55:16
chain of custody, meaning that the OTP
55:18
can deliver or a nurse or somebody,
55:21
anybody from the inside of the skilled
55:23
nursing facility can come pick up the
55:25
dose and bring it back to the
55:27
skilled nursing facility to administer it. Another
55:30
thing that came out in the new final
55:32
rule is something that's very clear, which is
55:34
that if you are a hospital, a long
55:36
term care facility or correctional facility who has
55:38
a DEA clinic or hospital license, which almost
55:41
all of us do, you actually don't need
55:43
to be an OTP to use methadone. You
55:45
can order methadone on your formulary from your
55:47
normal pharmacy, and you could dispense it to
55:49
patients. So if somebody
55:51
left the hospital on 120 milligrams and
55:53
you just knew this, you would just
55:56
continue them on their 120 milligrams without
55:58
ever interacting with an OTP system.
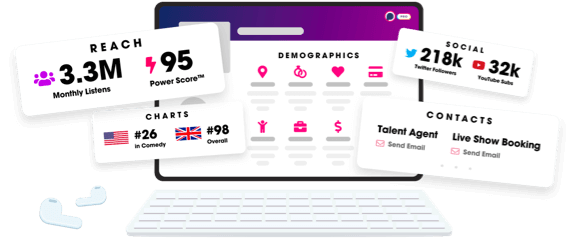
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
