Episode Transcript
Transcripts are displayed as originally observed. Some content, including advertisements may have changed.
Use Ctrl + F to search
0:04
Welcome to the Hope Podcast . My name is Jonathan
0:06
James and I'll be your host today . It is
0:08
really fantastic to be here
0:11
to talk about Hope Unmuted and
0:13
in this podcast we're doing a series on
0:15
women with bleeding disorders , and I'm really
0:18
excited to invite one of my
0:20
good friends and one of our board of directors , biven
0:22
Von Allman . Thank you so much for being here
0:25
with me today on the Hope Podcast . Very welcome , happy
0:27
to be here . Yeah , it's great to see you , as
0:29
always , and I should say , dr
0:32
Biven Von Allman , I apologize , but
0:34
you are a physician
0:36
and have been practicing
0:39
as an obstetrician , for I
0:41
won't say you're old , but a long time 30
0:43
years , 30 plus years , yeah
0:45
, and so really excited to talk
0:48
about today , specifically about women
0:50
with bleeding disorders and a little issues about that
0:52
. But I think there's a lot of education
0:54
that needs to happen and things that we're learning and we're
0:57
just trying to move the needle on . How do we advance
0:59
in that space , especially for women living
1:01
with von Willebrand's and maybe even
1:03
other bleeding disorders that just don't
1:06
know that they should be looking into these things . So I'm super
1:08
excited to dive into that topic , but
1:10
I just want to take a few minutes for people to
1:12
get to know you a little bit better , because it's
1:15
just you have such an incredible
1:17
background and story and so tell
1:19
us a little bit about where you're from and
1:21
also just kind of your journey of becoming
1:23
a physician and getting involved in the practice
1:25
that you're in .
1:26
I was originally born in Texas
1:28
and raised in five other states , ended
1:30
up here in Louisiana . I went to
1:33
LSU Medical School . Let's
1:36
see that was many years ago , 1983
1:39
to 1988 . I
1:43
went through residency at Charity Hospital
1:45
and all the charity hospitals from 1980
1:48
. Oh sorry , 19
1:50
. What years did .
1:52
I say so sorry yeah 1988
1:55
to 1992 .
1:57
And then I started in private practice and
1:59
I did obstetrics and gynecology for about
2:01
13 years and then I've been doing GYN
2:03
surgery for the last 30 plus years
2:06
and then retired Wow , so
2:08
yeah .
2:09
Well , I , you know , one of the things that I'm always inspired
2:11
by is your passion and your empathy
2:13
. I think a lot of times , um
2:16
so often , I know , for me I've had
2:18
, I have been a person that
2:20
has had white coat syndrome on more than one occasion
2:22
where I walk in and I just don't
2:24
know . You know , I get all high blood pressure
2:26
and everything else , and so sometimes that's
2:28
a result of you know , sometimes
2:31
you have expert physicians that are
2:33
maybe don't have always the best bedside manner
2:35
, but you are not that person . You're the
2:37
extreme opposite of that , and we have many
2:39
friends that you've helped through the years and , of course , you've helped
2:41
my family as well , and and
2:49
I've just , I've just always been so blown away at how much empathy and willingness to listen and really
2:51
hear what the needs are . I know , when I got to know you , you
2:53
were still working at a uh
2:55
, a hospital that was a nonprofit hospital
2:58
and , um , one of the reasons why you went
3:00
there is because you just cared for people so much . You couldn't
3:02
make a lot more money at a lot of other places . But you wanted
3:04
to really help the people that couldn't get help any
3:07
other way . And tell me a little
3:09
bit about your tenure there . I know that that was a passion
3:11
for you , but you worked on people that really had no insurance
3:13
, they had no ability to pay , they had no , no
3:16
ability . You , you really served the least of these
3:18
really in many ways , right .
3:19
Yes . Well , a lot of them
3:22
basically fell through the cracks , either
3:24
medically
3:27
, socially , economically
3:29
, and always had bigger
3:32
problems than they
3:34
really would like to admit to Just
3:37
learn to deal with it from the
3:39
perspective of bleeding to a point of
3:41
anemia that needed to be transfused
3:44
, sometimes
3:46
four or five times a year , and
3:50
really needed . They needed help and
3:52
the whole purpose was to try to help them out
3:54
. I mean , that's
3:56
why we're in medicine to begin with . Right Is to help
3:58
other people . It's not about
4:19
us .
4:19
So there's a main reason In those types of settings
4:21
and I've been in some of those hospitals and they are
4:23
really not easy to work
4:25
in it's lack of resources
4:28
, lack of staff , lack of medicine
4:31
, sometimes lack of all kinds of things , and so you
4:33
see , lack in every direction and to work in
4:35
that environment . How many years
4:37
were you there ? You were 20 , over 20 years . Yeah
4:40
, yeah , 20 years . And so to work in that kind
4:42
of environment for that long is almost like staying
4:44
in a perpetual sense of residency almost
4:46
in a way , I would expect , because
4:48
you're just Similar . Yeah , you're just working
4:50
in a space that just doesn't have all
4:52
the latest , greatest technology
4:55
.
4:55
Bells and whistles are out there .
4:56
Yeah , you don't have a coag lab that you can run
4:59
down and throw into a centrifuge and get an answer
5:01
right away . You have to wait for everything
5:03
and that's tough a centrifuge and get an answer right
5:05
away . You have to wait for everything and that's tough . But I know that you know working
5:07
with specifically with women with bleeding disorders
5:10
. One of the things we're learning is
5:12
that we hear stories of so
5:14
many people that
5:17
are , you know , I
5:23
mean , sort of a driving portion of that women specifically with bleeding disorders
5:25
is their menstrual cycle . Is can sometimes be one of the first
5:27
indications that there may be something wrong , that
5:29
they didn't get detected , maybe in some
5:31
other form or fashion . If you didn't have a , if
5:34
you didn't have , like , a family history in
5:36
a genetic sense , or you weren't aware of it because
5:38
someone else had gotten diagnosed in your genetic line
5:40
, you you may not have an awareness
5:42
. And one of the things we talk about a lot we just
5:44
, you
5:49
know , have been doing some education for von Willebrand specifically . One of the things
5:51
we learned about is the CDC reports . They estimate of almost
5:53
nearly 3 million people in the United
5:55
States could have von
5:57
Willebrand's disease , but only roughly
5:59
33,000 of those people are
6:01
even identified . I mean , they don't even know
6:04
where the gross majority of those . So that
6:06
tells me that there's a huge gap of
6:08
information that hasn't been . You
6:10
know of people that really need
6:12
to see where these problems are , so one of the things I wanted to kind
6:14
of ask you and I and I think
6:16
about a lot of times as an OB is
6:18
you know what
6:21
is a normal menstrual cycle timeframe
6:23
, cause I , I think we've seen some women that have had
6:25
timeframes all over the map , and and
6:28
so you know a lot of one of the first questions
6:30
that comes up is do you have longer
6:32
than normal ? menstrual cycles yes
6:34
, Well , I think most women are going
6:37
like well , I don't know , I just it's
6:39
my cycle you know like they don't really put that
6:41
two and two together , but since that's such an important
6:43
, maybe anecdotal way for the
6:46
average everyday person or female to be able to kind
6:48
of indicate what
6:50
is a normal time .
6:51
Sure , three days to seven days
6:54
. Anything after seven is really considered abnormal
6:56
. Okay , some women have been having cycles
6:59
for 10 days and two weeks and just been putting
7:01
up with it and thought that
7:03
was normal . Wow yeah
7:07
, anything that is in intermenstrual bleeding between
7:09
cycles is abnormal and
7:11
should be investigated . Anything
7:13
that is heavier than they say five
7:16
tablespoons , which is roughly 80
7:18
milliliters of blood
7:20
in a cycle . Now , most women aren't
7:22
going to measure 80 milliliters
7:25
of blood , so they
7:27
feel that if you're using
7:30
a pad or a tampon every hour
7:32
or you're having to use overprotection , that's
7:34
certainly excessive bleeding . And
7:36
some of those things don't get investigated from
7:38
the perspective of bleeding disorders because
7:40
, being
7:43
an OBGYN , one of the first things we investigate
7:45
is the actual organ that's bleeding the uterus
7:47
. Or we investigate the hormones
7:50
, or we investigate the ovaries , or we
7:52
investigate the lining of the uterus
7:54
. And I was just looking at a differential
7:57
diagnosis for abnormal bleeding and bleeding
8:00
disorders is a tenth down the line of
8:02
a number of 11 or 12 in the differential
8:05
diagnosis , so it's way down
8:07
the line .
8:08
So meaning that a doctor would probably
8:10
, if there was abnormal bleeding , say
8:12
, beyond that seven days or beyond that pad
8:14
per hour , whatever that measurement is we're
8:16
thinking about , if that's something that's
8:18
outside of the norms , they
8:21
would look at those other eight checkpoints before they
8:23
would Correct . And you said bleeding disorders are eight or nine , Eight or nine . Down the line forms they would look at those other eight checkpoints before they would
8:25
Correct . And you said bleeding disorders are eight
8:27
or nine . Eight or nine ?
8:28
down the line .
8:28
So they're going to go through a checklist in their own mind
8:30
as an obstetrician to go and say , well
8:32
, is it this , is it that , is it
8:34
this ? And they've got to basically through process
8:37
of elimination , eliminate eight things before they
8:39
get to a bleeding disorder , correct ?
8:41
Wow , right , in
8:47
other words , that's one of the last things that actually gets looked at , and sometimes it's already
8:49
to a point where it's it's too late
8:51
for them to actually be treatable
8:53
if they've already had an obstetric
8:55
emergency and possibly had a postpartum
8:58
hemorrhage or a surgical emergency
9:00
and possibly hemorrhaged post-operatively
9:02
or on the table .
9:05
I had a treatment center nurse
9:07
many years ago who is
9:10
retired and not
9:13
with us anymore . Actually , she passed away a few years
9:15
ago , but
9:19
she actually told me one time she said , jonathan , because if we ever had realized how
9:21
many people that had extended you know , abnormal
9:24
bleeding as women . What we're
9:26
finding is that we had potentially
9:28
thousands of them that had hysterectomies
9:31
before they were of childbearing
9:33
years because
9:35
they had bleeding challenges
9:38
. And if we would have just known that we could have given
9:40
them a little bit of factor or a little bit
9:42
of fungal-lipidinase protein or a little bit of treatment
9:44
, a little bit of von Willebrand's protein or a little bit of treatment , they could
9:46
have had a full life with all
9:48
of their faculties .
9:54
The education is way behind the process of treatment , which is amazing in 2024
9:56
to see the fact that we still are there .
9:58
We really haven't advanced a
10:00
lot .
10:01
Correct , which is where knowledge is
10:03
empowering to these people
10:05
. Yes , because if they don't have
10:07
and a lot of people
10:09
a thorough history
10:11
includes a family history A lot of people don't
10:13
have an idea of their family
10:16
history , maybe because of social
10:18
situations or maybe because they were adopted
10:20
. But most of the times
10:23
, if we make a diagnosis and somebody has a
10:25
real , strong family history , it points you
10:27
right to that disorder and the
10:29
need for treatment . That doesn't happen
10:31
the majority of the time .
10:33
Even shame , right ? I mean , sometimes
10:36
the limitation is that even within the
10:38
family unit , it's seen
10:40
as something not to talk about , so they just don't
10:42
want to correct . Seen
10:44
as something not to talk about , so
10:46
they just don't want to correct . That's amazing , correct and so this
10:48
. This is part of the reason why I know , as as a person in
10:50
advocating for people with bleeding disorders , this
10:53
is something that makes me really feel like man . We
10:55
got to get the word out because if
10:57
more people knew that
10:59
anything over seven days , anything
11:01
over a pad , an hour , anything like that , maybe
11:03
they would start to ask questions . Because if
11:06
that doctor has to go through eight different things before
11:08
he's going to investigate that , but
11:11
if the patient comes to you and says , hey , I'm
11:13
suspicious because of these reasons
11:15
as a treating physician , would
11:17
that make you want to maybe
11:19
look into that more ?
11:21
Absolutely I would . I would um rule
11:23
out the number one
11:25
through six things as quickly as
11:27
possible and then move on if there was
11:29
not an abnormality . You mentioned the word shame
11:32
. Not only shame , but it's also fear , for
11:34
some people Fear that they might find
11:36
something way worse than just
11:39
a bleeding disorder . They may not know about the bleeding
11:41
disorder , they may think cancer and
11:44
they may not want to come until it's to a point
11:46
where they've had to receive a transfusion . I mean , if
11:48
you see somebody that's been in the hospital and had to receive
11:50
transfusion two
11:53
, three times in a period of five
11:56
, six years , that should be a red light . That
11:58
should go on . Now , the other issue
12:00
is that you know making the referrals to the doctors
12:02
and sometimes those are pretty long waits
12:04
to hematologists , oncologists , and
12:07
they don't want to wait that long or they
12:09
won't wait that long or maybe it's even in another
12:11
city .
12:11
That's really really uh , too
12:13
hard for some of my patients to
12:16
be able to get to , absolutely , absolutely
12:18
it's very interesting
12:20
I really thought about those hurdles being things that
12:22
we have to , yes , consider when we're
12:24
trying to encourage
12:26
people to provide solutions . One of the there's so
12:28
much oh my gosh , we could probably talk for hours
12:31
about just rural health , because so much of
12:33
what work you've done in your career has been
12:35
sort of targeting , bringing
12:37
resources to people in rural settings , and , and
12:39
that's such a huge need . But I
12:42
don't think we can underestimate how
12:44
much just that travel , even even 30
12:46
minutes an hour away , much
12:48
less wait times to get into a specialist all
12:50
those things create hurdles . So
12:52
one of the things that I think is also important is that , and
12:55
one of the things I'm so grateful for you , um
12:58
, getting involved with hope and being a part of our board
13:00
of directors , and we'll we'll dive into some of that
13:02
in a little bit too , but I I wanted to , you
13:04
know , just say that one of the things I'm so grateful for
13:06
is that I do believe that more
13:08
education could be provided to
13:10
obstetricians as a whole that are practicing in many
13:13
different communities . Maybe , maybe there's a way
13:15
we can continue to expand there too . But
13:18
you know in in your experience
13:20
, and I think about you doing so much on the surgical
13:22
side were there ever times that
13:24
you were doing surgery on somebody , that you
13:26
had accessibility and you saw and observed
13:28
concerns of maybe bleeding , that you
13:31
thought , man , maybe I should look into
13:33
this .
13:33
And then you did look into it and found out it was
13:35
von Willebrand's or it was some other kind of bleeding
13:37
problem , Absolutely , there were several
13:39
times I
13:48
never had the ability to be able to follow up with these patients , mainly because
13:51
they wouldn't come back , I mean they would not go on . I
13:54
actually had a lady that came in and gave me a family history before she actually
13:56
had surgery . Thank goodness , because she told stories of her mother and the scenario
13:59
that happened with her in the operating room and
14:02
she almost didn't make it Wow
14:04
. And so we were able to give her factor
14:07
before we did the surgery to help Right
14:09
, and you're well aware of that . With bleeding disorders
14:11
, you know a factor . I mean a lot of people think hemophilia
14:14
. There's no way they're never going to have any , any
14:16
operation because they don't know about
14:18
the factors , they don't know about the ability
14:20
to pre-treat and to be able to make it a safer
14:22
environment for them to have surgery Right
14:25
. And that happened a lot years ago when
14:27
I was in training and right out
14:29
of training .
14:29
Wow , well , truly , I mean , with
14:32
the way you know product
14:34
and availability and all of these things , with
14:36
the right information , bleeding
14:39
disorders is a problem that can be resolved
14:41
. It's something that can be solved , it's not
14:43
something that is so . I
14:45
mean , I think that there's a fear with . I mean , 30
14:48
years ago , 40 years ago , there
14:50
really was such a very , not
14:54
just a lack of knowledge , but there was also a lack of availability of medication
14:57
to be able to address these issues . Now
15:00
we thankfully in the world today
15:02
, especially in first world countries , we pretty
15:04
much have accessibility if we can know
15:07
about these things ahead of time . And so now the biggest challenge
15:09
is actually that knowledge gap . It's actually about
15:11
helping people understand , and
15:14
you know , especially Von Willebrand is one of those things where
15:16
it's 50-50 . Some are men
15:18
, some are women . It's not like
15:20
in hemophilia , for instance . We experienced
15:23
that , as I have severe hemophilia . Historically
15:26
that was considered just a male dominant disease
15:29
.
15:29
We're learning now that's not true either .
15:31
And so so we're trying to understand
15:34
and , as we're learning , I think it's
15:36
important that we get this information out to so many
15:38
people because , really , I think the patients
15:40
in many ways are the people who might be suspicious
15:43
that these are things that they might have trouble
15:45
with . If , if you
15:47
empower yourself with information , going
15:50
to your treatment plan with
15:52
your physician to say , hey , these are things I'm concerned
15:55
about it could like you said , that lady
15:57
that came to you ahead of time it could actually
15:59
provide you the information you need
16:01
to to do some investigation
16:03
in that direction . And I think , as an OB , like we
16:05
, we think very often in in
16:07
hemophilia it's like , well , you just got to go
16:10
to the treatment center and you got to go see a hematologist , but
16:12
, but a lot of times the wait lists are very long . They're
16:14
also very , in very specific places
16:16
that can be difficult to get to , and maybe
16:18
the OB is the place where you might
16:20
be the most common place to discover
16:23
that , especially for women . And
16:25
, uh , I just think that if
16:27
, if we get the message out to patients
16:29
this is an area that if they
16:31
, if they have the , if you're suspicious , and
16:34
if you're listening to this podcast and you're thinking , man , oh
16:37
my gosh , like five tablespoons , eight tablespoons
16:39
of blood . Yeah , that's me every month . Maybe
16:42
it's worth asking some questions , Absolutely
16:44
.
16:45
Absolutely . If there's any doubt , ask questions and
16:47
if the questions are receptive
16:49
, or if the physician
16:51
is receptive to your questions , great
16:54
, get him to push the ball forward . If
16:56
that means a referral , if that means doing some
16:58
blood tests , if they can do it , you have
17:00
to try to make that available . Yeah , if they can do it , you have
17:02
to try to make that available . Now
17:05
, a lot of people will how should I say this
17:07
If they don't know about
17:09
the actual disease process , kind
17:11
of stray away from it because fear that they
17:13
don't know anything about it and
17:15
it's not treatable for them , it's
17:19
not something that they can treat . And years ago , I
17:21
mean when I first was training , I mean hemophilia
17:23
was . I mean basically people thought , well
17:26
, that's just pretty much a death sentence . You
17:29
know they're going to bleed to death if you don't , if
17:31
they have a problem , and that's still I
17:33
mean I hate to say this in some social
17:36
areas probably still thought
17:39
of as the same way Interesting yeah
17:41
.
17:41
Which is totally false . Absolutely , but
17:43
we don't , but they know no better . Interesting , which is totally false , absolutely
17:45
. But we don't , but they know no better . But they know no better , right , in
17:47
medical school , I mean , you know , correct me if I'm wrong , but
17:50
I understand . It's like you're going to be . A
17:52
very small portion of your training is even
17:55
going to explain a definition of these
17:57
things , right ?
17:59
Right , correct , and unless you specialize
18:01
specifically in hematology , hematology
18:04
, oncology , you're not going to get the training
18:06
in that . Because even if
18:08
you do internal medicine , there's so many other
18:10
things that they have to
18:12
know about . I mean , they're going to know a little bit about
18:14
it . They may know more about it than
18:16
, say , a pediatrician
18:20
, they may know more about it than
18:22
a general surgeon , but realistically
18:24
we don't specialize specifically
18:26
in learning about that until it's something
18:28
that we have to deal with .
18:30
Yeah , which is hard . That's
18:32
so interesting . At what point do you think somebody
18:35
might need to reach out
18:37
to a treatment center , would they ? Would they
18:39
go to their OB first and
18:42
ask that question and then their OB refer them to ? Should
18:44
they go to the treatment center right away ? What
18:46
do you think is the best thing ? Because if
18:49
they go to somebody who's not educated
18:51
on that issue , I
18:53
guess my concern and what we've seen happen sometimes
18:56
is sometimes that's just brushed off and
18:59
kind of almost dismissed
19:03
, because everybody doesn't have the luxury of being
19:06
in relationship with somebody as amazing as you , that
19:08
you're going to take that information to heart , you're
19:10
going to investigate , you're going to you , but not
19:12
every physician is like that , and so I guess the question
19:14
is like , if there's
19:16
a dismissal there , should they still keep
19:18
pushing and maybe look for somebody
19:21
in hematology , or should they wait
19:23
on their obstetrician to make that ? Should they go to the PCP
19:25
? I don't know .
19:25
You know what do you recommend ? I would say that they need to get
19:27
a second opinion from another if it's a primary
19:30
care provider , if it's a family practitioner
19:32
or if it's a
19:34
hematologist . That kind of dismissed them and
19:36
they never did any testing on it . If
19:39
you get to that point and second or
19:41
third opinions , you're not getting anywhere . If
19:44
the treatment center is the place where they can
19:46
get evaluated , that
19:48
would be the place to go . That's what I'd recommend . I
19:50
didn't even know about hemophilia treatment centers
19:52
when I was trained .
19:54
And you were ordering medications in
19:56
some occasions for surgeries , even for
19:59
these types of issues , absolutely , but you didn't even know
20:01
to refer to that . No , yeah , and
20:03
that's right here no education , yeah , but you didn't
20:05
even know to refer to that . No , yeah , and that's right here . No
20:07
education for that ? That's amazing . Well
20:09
, there's so much more work to do . I do feel like and I'd be curious
20:11
to know your thoughts on this how important
20:14
is the
20:16
patient themselves , how important
20:19
is their
20:21
determination to
20:23
find answers to
20:26
getting an actual solution ?
20:28
Very If they continue
20:32
to have the problem , it continues to be
20:34
a situation that is inconveniencing
20:37
them . It's very important for them
20:39
to push that ball forward , so good yeah
20:41
, and
20:43
they may run up against egos
20:46
or run up against people that don't want to do
20:48
anything about it . Continue to seek out
20:50
somebody who cares
20:52
.
20:53
That's good . I heard you say one time in one of our conferences
20:56
you said you know ? I said if you don't get
20:58
what you need in a first opinion , get
21:00
a second opinion . If you don't get a second opinion , get a third
21:02
, fourth , fifth , sixth , seventh opinion .
21:04
If that's what it takes , yeah .
21:05
Right , I love that because it's so
21:07
, and I , you know , as
21:09
a person living with a bleeding sore on my end
21:11
, I have been in those situations where
21:13
I felt like I wasn't being heard . I
21:15
felt like I wasn't being listened to . How
21:22
being listened to ? How does somebody stay inspired
21:25
to keep ? Because I feel like that there's a fine line . We talk about this a lot in advocacy is . I think that there's a fine line between being um
21:28
, an activist and
21:31
and and an advocate
21:33
. I think that you can almost lean
21:35
into when you feel like you're not being heard . You can almost lean
21:37
into a place of being adversarial and that's
21:40
not , that's not going to produce anything either
21:42
, no , and so I think there's
21:44
a fine line in that . But you
21:46
know , one of the things that I've wrestled with a lot
21:48
is how to inspire people to
21:50
, to keep to , to stay
21:53
inspired and and
21:55
to keep asking questions , to stay curious
21:57
. You know , right , and and
22:02
you had to face that as a physician too , because you were not trained to be a hematologist
22:04
, correct . So how did you stay inspired in
22:06
your practice , in your career , to be able
22:08
to stay , start saying let me get
22:10
curious about things that I will . Maybe I wasn't
22:12
trained in .
22:13
Right ? Well , many , many of the aspects
22:15
of what the patient will come in with
22:17
when it's not something specifically in
22:19
our specialty . If
22:22
you're not listening , if you're not paying attention
22:24
, you're not going to pick it up , and I
22:26
never forget that . I was told that if you listen
22:28
to the patient , tell
22:31
their history , they'll tell you the
22:33
diagnosis . At least 90% of the time
22:35
, no-transcript
22:50
. We all have things going on at work . We all have things
22:52
going on at home . We all have situations
22:55
going on outside of work , right , and
22:57
if you're not being listened to as a patient
22:59
, then you need to go and find somebody that's
23:01
going to listen to you and going to continue
23:04
to help you along with that , trying
23:06
to make the diagnosis or find out what
23:08
the problem is . Yeah , if you're not satisfied
23:10
, that's a good point . That's a good point
23:12
. And
23:19
it's hard . You can't be how should I say ? They can't be very negative or pushy bitter . They just
23:21
need to try to emphasize the fact that they would like to really
23:23
know why they're having the problem .
23:25
Stay focused on the problem , correct
23:27
Nothing else . Don't get distracted
23:30
by the emotions or the fear , or
23:32
the shame or the which can
23:34
be hard , which can be so hard If you've been dealing
23:36
with it for years and especially when you're suffering , because
23:38
this is not , you know , one
23:41
of the things that I think is so important , and I would think anybody in the nonprofit
23:43
world or you know like , even
23:45
even in the work that you did within nonprofit hospitals
23:47
. But your whole premise is
23:50
, your whole life is really wrapped
23:52
around trying to reduce unnecessary
23:54
suffering and at the same
23:56
time , the rigors of schedules
23:59
and and all of that stuff can put a lot
24:01
of stress , and the same is true for the patient . The patient
24:03
a lot of times can be in a situation where they're they
24:06
had to take hours off of work to even
24:09
show up to an appointment and now it's
24:11
going to take another 30 minutes for you to have a discussion
24:13
or a conversation and sometimes , if you're not getting
24:15
feedback , it can be really , really , really painful to
24:17
keep that momentum . But I
24:20
just want to encourage people who
24:22
may be listening to this thinking oh
24:24
my gosh , like I've noticed this tendency
24:26
and I've noticed this problem , and I almost
24:29
died in childbirth or , you know , I
24:31
almost had these problems where I had a . You know , I was
24:33
very depleted , almost needed a transfusion . Maybe
24:36
you should ask questions . Maybe you should
24:38
keep asking questions and
24:41
not just be satisfied with that . Maybe you did have
24:43
a family history , but there was never
24:45
a label for it . Well , that's okay
24:47
, Keep asking questions
24:50
, because we're all constantly in a state of learning
24:52
. I think sometimes people I talk to so
24:54
many people out in the American public , so much , it's like well
24:56
, technology is so good today and AI
24:58
is so great and we have all these answers
25:01
now it's like , but we still don't know everything . I mean
25:03
, in so many ways it's unfathomable to think
25:05
that we're in a state
25:07
of you know of this
25:09
universe where we can't , we
25:11
really don't know all the answers , but
25:14
we really don't . There's still so
25:16
many things that are unknown yet right
25:18
?
25:18
Yes , I mean , you said 3
25:20
million people with von Willebrand .
25:22
Right .
25:22
Only 33,000 diagnosed Right
25:24
. What percentage of those people that
25:26
have it don't know Right and their family
25:29
doesn't know that they have it Right . And
25:32
people that are even close to the
25:34
bleeding disorder community find
25:36
out . Oh , after I finally started
25:38
learning about bleeding disorders , somebody in my
25:40
family actually had this
25:42
, so their eyes are open to it and
25:45
it's just not something that we pay that much attention
25:47
to , and especially in the medical
25:49
profession . Unless you deal specifically with
25:51
the bleeding disorder community , it's
25:53
not one of the top priorities on the list , like
25:56
I said that differential diagnosis is way
25:58
down there On metarrhagia , the
26:00
heavy bleeding or the long
26:03
prolonged periods . I
26:05
think it's eight or nine on the differential
26:07
diagnosis . On metarrhagia , the heavy periods
26:09
, it's nine or 10 on the differential
26:11
diagnosis out of 11 to 12 diagnoses
26:14
. Almost at the bottom yes , wow
26:16
. Before it's even checked off the list to
26:19
look into or investigate Wow , that
26:21
it's even checked off the list to look into or investigate , correct Wow . That's amazing . And there's so many things happening , whether
26:23
it's postpartum hemorrhage , whether
26:26
it's postpartum hemorrhage to
26:28
death , whether it is intraventricular
26:31
hemorrhage on a baby that's
26:33
born vaginally and
26:35
the mom was never diagnosed with any type of
26:37
bleeding disorder , and yet the child , a male
26:39
child , comes out with hemophilia . Right
26:42
, that could have been prevented , right , you
26:44
know post-operative hemorrhage
26:46
, right , or not making her off
26:48
the table from surgery .
26:50
Right , I would argue that this obviously
26:52
because of the gap again going back to those CDC
26:55
numbers 30,000 that are diagnosed
26:57
.
26:57
Three million .
26:58
Three million that are you 3 million that are anticipated
27:00
? I think , because of that gap , it's
27:02
very logical to me
27:04
to assume that we have
27:06
some , that
27:09
there's many , I mean , according
27:11
to those numbers , there's millions of people in
27:13
the United States living with this problem that literally
27:15
don't know , and so it's
27:17
worthy of us to do this Now . For women
27:20
in this case , obviously , the menstrual
27:22
cycle is happening every month , and that could be
27:24
an indication . But in
27:26
some cases , what if you have other comorbidities
27:29
, like , say , for instance , you have , uh
27:31
, you're not having normal cycles at all ? I
27:33
mean , for instance , I have two daughters both
27:36
both are you know , of the age where they're having
27:38
their menstrual cycles , and they had other
27:40
issues , like PCOS , that prevented them
27:43
from having cycles for a period of time . And
27:45
so that was the first question that was
27:47
asked . Well , when they said
27:49
, well , I haven't had a cycle in three months , or
27:51
something like that , well , oh , well , then you don't have a bleeding disorder
27:53
, which later we found out was not true , they
27:55
actually both had a bleeding disorder , and
28:02
so I think it's easy to talk about the cycle as being a potential problem , but you
28:05
could have that same person that could be in childbirth . You
28:07
brought this up and that's where it raises
28:09
its ugly head , is in the middle of a trauma
28:12
, correct , right , correct . And
28:15
so what do you do ? I mean , if the doctor's not expecting
28:17
it , if the staff is not expecting it , if you're not in a hospital
28:19
that knows how to look for that and
28:22
you don't have enough ? I mean , there's
28:24
far more people at risk of this . I
28:26
think that's why we have potentially millions
28:28
of people that are at risk for this that just
28:30
haven't heard , they just don't know .
28:31
We've just talked about von Willebrand's . What about hemophilia
28:33
? I mean , when I was going through residency
28:36
, it's only males that have hemophilia , that have bleeding
28:38
disorders . Now we know that there's females
28:40
, that's right . So I mean , when
28:42
you get to that point where it's an obstetric
28:45
emergency or a postoperative emergency , that's when the
28:47
fire drill starts , that's right . Even
28:49
if the fire is put out , that
28:51
doesn't mean that you shouldn't
28:53
continue to work up the patient . That
28:55
should be a red flag right there , right ? But
28:57
unfortunately that doesn't happen all the time . Right
28:59
? And if the patient is in that situation
29:02
, they have to continue to inquire .
29:04
Yeah , the patient's got to be in the driver's
29:06
seat . Absolutely , they have to be the one to put
29:08
the pressure on and ask questions from
29:10
every direction . It can't just be , you know
29:13
, I think that there's a tendency for all of us to
29:15
want to . You know , um , I
29:17
know , I know . Part of the white coat syndrome , for instance
29:19
, is something where you're
29:22
fearful when you go into a doctor because you haven't been
29:24
trained in medicine as a novice . I'm
29:27
going in and I wasn't trained to be a doctor
29:29
, so I don't know . There's a lot
29:31
I don't know . You know , at the cellular level
29:33
, I could not tell you how an enzyme interacts with a
29:35
protein , ends up with a . I don't know . You
29:37
know what is a gene compared to
29:39
a red blood cell ? I , you know what
29:41
is a gene compared to a red blood cell ? I , you know , sure , you know . But the point
29:43
is is that we don't really , you
29:45
know , while , while , while
29:48
I think it's easy for us to focus and say we're
29:50
not the experts , that
29:52
individual person is still living with
29:54
their own flesh and blood , their own body
29:56
, I mean a lot
29:58
longer than any researcher will
30:00
be able to see that any investigator , any
30:07
doctor , any treating physician , and that's not a knock on the profession . That's just to say
30:09
that you may have things that you notice within your own life
30:12
that raise their head at variable times
30:14
, like , for instance , my daughter . One time when
30:16
she was very little , she fell
30:18
and she hit her lip
30:20
on the stairs and it busted her lip
30:23
. Well , don't you know the doggone thing
30:25
like bled for like three days
30:27
and we couldn't get it to stop and we even
30:29
asked the question is this , possibly this ? At the time
30:31
, the predominant thinking was not that
30:33
cause girls can't have it . But it
30:36
wasn't because we weren't asking questions
30:38
, but we didn't continue to
30:40
keep the pressure on . And so a
30:42
decade goes by , there's other problems
30:45
and now she has some joint damage
30:47
as a result of not asking those right questions
30:49
. And I can't blame myself entirely
30:51
to say that it's 100 . I can't walk around with the
30:54
shame of that and guilt of that . I've got to be careful to manage
30:56
that emotion in my own heart . But at the
30:58
same time I really can't blame
31:00
the medical physicians that
31:03
we're looking at at the time , either because they didn't
31:05
have the information . But it's incumbent
31:07
upon me as the parent or as the person
31:09
living with that I've got to still keep
31:11
asking questions if I see these trends , because
31:14
I'm looking over decades of my own
31:16
personal life and I
31:18
don't think we should downplay
31:20
that as a non-physician .
31:25
Issue Issue Right , and you live
31:27
with yourself every day . Right , the doctor sees
31:29
you once every year , once every six months
31:31
. Right , if it's an OBGYN
31:33
, they may see them once during their pregnancy
31:35
. See them once a year after then for pap
31:37
smears or annual exams Right , for
31:40
maybe five , ten years . Right
31:42
, if it's a really long time , it could be 20
31:44
. Well , by then you should have an idea . But Well
31:46
, by then you should have an idea . But then you have to remember this
31:48
also , jonathan the things that you've gone through with hemophilia
31:51
bring a tremendous amount of
31:53
pains , burdens
31:56
, battles that you have to deal with , and
31:58
sometimes it's hard for the patient to remain
32:00
focused , to ask the right questions over
32:02
and over and over again because of what's going on in their
32:04
life . So that's really hard
32:06
.
32:10
That is hard , which is why we need organizations like Hope to help encourage , and
32:12
that's one of the things I love about what we do is we
32:14
, we try to do . Moments like this
32:16
, we try to do educational opportunities
32:19
. We try to help empower people because
32:21
, at the end of the day , like it is
32:23
a long , it's a lifelong road . It's not
32:25
just a long road , it's a lifelong
32:27
road and it's one
32:29
that really does . There's lots of ebbs and flows
32:31
and there's lots of things that occur
32:33
over the over decades and decades of a lifetime
32:36
and and very likely you're
32:38
going to get tired You're going to need some encouragement
32:43
that you've
32:45
been such a huge , really
32:48
answer to prayer for me personally as being
32:50
a part of our team , because when
32:52
you came onto the board of directors , we were just
32:54
starting to really step out
32:56
into how can we really educate
33:00
people on this issue of how
33:02
women are impacted and
33:05
try to really make some strategic change in that
33:07
area . Tell me a little bit about
33:09
, like , what drew you to hope , what made you
33:11
want to get involved with hope and and
33:13
and . What is it that you're excited about as
33:15
you look into the future , of what we could do as a , as
33:17
a group and as a team ?
33:19
The heart of hope is really what drew me in
33:21
. I'm just so humbled
33:23
to be part of it , be on the board , because
33:26
when I first initially
33:28
was approached about it , it was like I didn't
33:30
have time to do that . I was busy with other
33:32
things going on in life . Then , when I realized
33:35
what the heart of hope was , it's I
33:37
don't have time not to do that . Y'all are
33:39
here strictly for the patient . You're
33:41
here to help people in crisis . You're here to
33:44
help people in need . You're here to educate people
33:46
. I
33:48
would say at this point in time , you're probably
33:50
pushing the ball forward more with women's
33:52
health than any other organization
33:56
that I know of . From the perspective of bleeding
33:58
disorders , that's
34:04
like number one in my eyes , because
34:06
that's what I take care of . Women
34:09
are awful , awful
34:11
, a lot how
34:14
should I say this ? Underappreciated and
34:17
not treated with the same especially
34:20
racially , some women and
34:22
not treated with the same respect and the same
34:24
amount of interest
34:26
that some other people are treated with
34:28
. So I took care of an awful
34:31
lot of those women and just
34:33
to have them come in and feel like somebody
34:35
was caring about what
34:37
was going on in their life , somebody was listening , somebody
34:40
wanted to help them . That's what
34:42
you guys do all the time , a hundred percent
34:44
. And that's what drew me in . And then
34:46
, when I said , okay , I
34:48
give , I'm going to be a member , I
34:51
sat in here and I thought , why
34:53
am I even here ? Why did they even ask me ? I'm
34:57
not even qualified to do this . Oh my gosh
34:59
.
34:59
But then I realized no , I wasn't qualified
35:01
.
35:01
I was called to do this , wow . And
35:04
as I was called to do this , then he's going
35:06
to give me the qualifications that I
35:08
need . That's so good , so that was the beauty
35:10
of it . And then I just see the just expansion
35:13
of the people that y'all are reaching . Yeah , and
35:15
it's not because you
35:18
want it to be about you , you
35:20
want it to be about hope , you want it to be about
35:22
the people . That's right . That's right .
35:26
That's why we're all here is for others . That's so good . Bevan , oh my gosh , I
35:29
yeah
35:31
, I can't even begin to
35:33
say how grateful I am for your
35:36
involvement , because it
35:38
it's not just a project for us
35:40
. I and I think that that's what's important
35:42
for people to understand is that it's
35:44
not we live this number one
35:46
. I mean I live it personally . You've seen
35:48
so many of the people that we you know , so
35:51
many of our employees , so many of the people that are involved , so
35:53
many of our volunteers . I mean it's like it
35:55
affects us at every , the fabric
35:57
of who we are , not just resources
36:09
and and expanding , you know , the possibilities of treatment
36:11
and all of those things , and really , truly advocacy work for women
36:14
with bleeding disorders is it's not like a trendy
36:16
thing . We're trying to pick up and I think that
36:18
that's something that's unless you're involved
36:20
really deeply , you probably don't know
36:22
that , because some of these things can feel
36:24
like they're a little bit a little bit like
36:26
oh , everybody's talking about , let's just talk about it . You know , and
36:29
I would say that there's a lot of folks out there
36:31
in the bleeding sort of community that really are
36:33
doing a lot , rolling up their sleeves , committing
36:36
to trying to make change , committing , trying to improve
36:38
, which is so heartwarming
36:40
it really is , and so , but for
36:42
hope , it's not something for us that we're just
36:44
trying to like , adopt as like just
36:47
an extra thing that we're doing to us
36:49
. This is central to what we do and
36:52
, uh , we're here for the disenfranchised entirely
36:55
. We're here for the people that don't . We
36:57
want to meet unmet needs . We're not trying to
36:59
duplicate what everybody else has done . We're not trying to just
37:01
jump on a bandwagon . Even this is something
37:03
for years upon years that we continue to
37:05
layer upon layer as we learn . We want
37:07
to pass that information along . You
37:10
said earlier , knowledge is power , like that I
37:12
mean truer words , right , we never spoke , I mean it's
37:14
. It really can be empowering
37:16
when you have the knowledge . And my
37:19
hope is is that people listen to a
37:21
conversation like this or they look at other resources
37:23
and they think about okay , maybe
37:26
, maybe I can get the courage up to ask
37:28
my OB like am I maybe
37:31
above average ? Am I bleeding more than
37:33
normal ? And I hope
37:35
that one day in time I will be able to look
37:37
back and say , oh my gosh , now
37:40
we have 2 million people that are diagnosed
37:42
, not because I want to see just everybody
37:45
have a bleeding disorder . It's kind of like pointing
37:47
to ministry of insurance . You know , you just , you don't really necessarily
37:49
wish it on anyone , but at the same
37:51
time , it's like that knowledge gap
37:54
has got to close , and I think it starts
37:56
with the patient community . At this point , in
37:59
an ideal world , I'd love for everybody
38:01
in every medical school to be educated
38:03
up to the hilt on these things . But you know what ? There's
38:05
thousands of rare diseases I
38:07
talked about . You've heard me say this at a lot of our conferences
38:09
, but it's like it's still amazing to
38:11
me to think that there was , like what ? 7,000
38:13
rare diseases diagnosed . A very good situation
38:15
in the sense that we have a lot of resources that maybe other communities
38:18
don't . So
38:35
we hope to help with this . We
38:37
hope to help with even other rare and ultra rare
38:39
diseases that don't have any resources
38:42
or support . But I want people
38:44
to know that what we're
38:46
hoping to do is really commit to
38:48
this for the long haul . It's not just a project
38:50
. Long haul and not just . It's
38:53
not just a project .
38:54
It's not just a trendy thing . It's something that's central to who we are . That's
38:56
another thing about the heart of hope . It's out to help those who can't help
38:58
themselves , and you're always looking for
39:00
somebody else to help , which
39:03
is just the amazing thing to me , which
39:05
is so humbling to me . I look at y'all
39:07
, especially some of the people that
39:09
I know have hemophilia
39:12
and are getting treatment , and I think to myself
39:14
and they go on every day and continue
39:17
and don't gripe
39:19
about it , don't moan about it , and
39:21
look at our lives , those people who aren't
39:24
affected , and yet we're going to complain about
39:26
something or grumble about something , and I'm thinking
39:28
we have it so good compared
39:30
to y'all , and y'all are just going
39:32
on and on . And I
39:34
think to myself , after 34
39:36
years of doing what I've done , all
39:39
the possible treatments that we've had , whether it's
39:41
hormones , whether it's surgery , whether
39:43
it's aggressive surgery , and
39:46
people are still having these problems . We're
39:49
not curing them . We're not taking care of the root
39:51
issue . We're just taking care of the symptoms
39:53
. We need to get to the root issue , to the
39:55
deeper root of what's going on , to
39:58
actually take care of the patient themselves
40:01
. Because , even if they've had bleeding
40:03
issues and you've taken care of their bleeding
40:05
problems from the perspective of some hormonal
40:08
treatment , or they break through
40:10
and then you've had to do surgery minor surgery , and then
40:12
you've had to do major surgery . What
40:14
happens after the surgery is over ? Are they going to have something
40:17
else going on if they truly have an underlying
40:19
problem ?
40:19
Yes , they will .
40:20
Did we really take care of the root of the problem
40:23
?
40:23
No , that's what we need to get to
40:25
, which is why it's incumbent upon the
40:27
patient population to continue
40:30
to ask the questions Because , honestly , it's
40:32
a point of diminishing returns . You can't expect
40:34
every single doctor you encounter to be the
40:36
most expert at every single thing . I
40:40
don't go to my cardiologist
40:42
to see how well my
40:45
hemophilia is doing .
40:51
There's just too much information that we all know .
40:53
There's no , possibly every person , every specialist
40:55
can know everything , and so
40:57
, um , you know , I do think it's incumbent
40:59
upon us to to educate ourselves
41:02
. What to that end
41:04
? What ? What do you think people
41:06
should do if they want to educate
41:08
themselves ? If they , if they're suspicious of these
41:10
things being potentially probably , for
41:13
instance , men that have von willebrand's
41:15
disease , it's a very common symptom
41:17
that they would have excessive nosebleeds
41:19
. That might be seasonal . They might be seasonal
41:22
, but they , they bleed more than normal from
41:24
a nosebleed . Sometimes people have bleeding in their gums
41:27
and their teeth . They have , they
41:29
have bruising . That occurs , they just
41:31
don't Unusual bruising right
41:33
. It feels like it's more common
41:36
than it would be maybe their friends , Right ? What
41:38
would you do to encourage maybe a guy
41:40
or a girl who might suspect that
41:43
there's something going on here that might be different
41:45
? How would you encourage them to get to
41:47
the education ? Because
41:50
I think that that's that's still a question mark out there . I mean , we're
41:52
trying to do what we can with maybe online stuff , but what
41:54
do ?
41:54
they do . Well , I mean , as we all
41:56
know , the internet's right there at our fingertips . I
41:58
mean people go to that all the time Search
42:01
out somebody that has a problem or
42:03
has the problem , or a
42:05
organization that deals with those specific
42:08
type of problems , and one
42:10
like Hope . They're more than willing
42:13
to help the patient and educate
42:15
the patient and give them information and
42:17
direct them in the right direction . That's
42:19
right , which is another super positive
42:22
thing about the heart of Hope yeah , you're always willing
42:24
to help people out . Yeah , in
42:26
more ways than just the ones that are
42:28
in crisis , people that are inquiring
42:30
. That's so true . That's what this is all about .
42:32
That's so true . We
42:36
were talking about this earlier about how we have a staff member
42:38
here who came to work and
42:40
really they came with a deep
42:43
amount of professional background and all kinds of things
42:45
and they got here and they started to get . They
42:48
had known that some of their family members
42:50
might , if they ever had to
42:52
have a surgery or some kind of extreme thing happened , they
42:54
might need something , and they
42:56
weren't . They didn't know what it was , and then
42:59
they started to learn through some of our online things
43:01
and they were like wait a minute . They went back
43:03
to their family members and said , what
43:05
do you have again ? And one of them knew and one of
43:07
them didn't know . And
43:10
and one of them didn't know and one of them started to . Well , it turns out she's a female
43:12
that has Von Willebrands and she
43:14
just had to have a double knee replacement and
43:17
she's only in her late
43:19
forties , early fifties and
43:22
you know there's a suspicion that
43:24
maybe if she had had treatment for him . Well
43:27
, this employee started handing
43:29
them the information he was learning and he's
43:31
like , oh my gosh , like how
43:33
, why didn't we know all this before ? But it took him
43:35
working , you know , in the environment to even realize
43:38
oh my gosh like , and
43:40
that's the piece that I hope to solve someday . Like I
43:42
, you know , as an organization , one
43:44
of the things that we've had a passion for , obviously , is
43:47
serving the people that know what
43:49
the problem is , but I never
43:51
actually , you know , I've now been
43:53
, you know , working as an employee
43:55
of Hope . I mean , my wife and I started the organization
43:57
15 years ago , but as an employee , I've
44:00
been here for 11 years , I think we
44:02
just said and so in
44:05
that timeframe , I never imagined
44:07
that we would be doing campaigns and trying
44:10
to reach out to maybe mass
44:12
population , not just these
44:14
small niche communities , and
44:17
it is amazing to think about
44:20
the future of what we could be doing
44:22
. We need an army of people to get educated
44:24
so that we can infiltrate every
44:26
community . We can infiltrate every , and
44:28
the internet's a good place to start . People can
44:30
join an online educational
44:33
session and listen in . We
44:35
just did this Von Willebrand's conference . We're
44:37
planning on doing that for every year going forward . But
44:40
those online things you could invite a neighbor
44:42
, you can invite a friend , you can invite somebody that said
44:44
you know , I think maybe there's something
44:46
I know about that . Well , maybe invite them . You know , I think maybe there's something I know about
44:48
that . Well , maybe invite them . You know , get involved . You know we have our hope conference
44:51
coming up in the fall super exciting . We have a few scholarships
44:54
that people can get to travel . But even if we can't , you
45:00
can access that same conference online . Maybe they can come and listen to some of those sessions
45:03
to understand , to get some of the language , to get some of the learning about , maybe
45:05
, what questions to bring to their doctor or
45:07
their clinical setting . My daughter , my
45:10
oldest daughter , actually got her first pretty
45:14
educated on how this stuff works , and it was genetic
45:18
. So we're looking for the same thing . We'd
45:20
gone to specialists and it's probably
45:22
not whatever , but nobody had really drawn blood
45:24
work . Well , I was able to get my PCP
45:26
, my family doctor , our
45:29
primary care physician , to actually pull the
45:31
blood work and they were like , yeah , sure , we'll pull
45:33
it . We can't maybe diagnose it necessarily or provide
45:35
treatment . We can actually look into it . Well
45:38
, sure enough , there was the answer
45:40
right there and she's like , oh , this is definitely what that
45:42
is . So then we had information to
45:44
take to the specialist and say , oh , this
45:46
is what . And
45:54
then it was a different story after that . But I just think that's what
45:56
I'm excited about , about what you and I get to do as as part of this really movement
45:58
in a way is to really bring not only bring people together to
46:00
learn and grow and support each other . That's super
46:02
huge . I , I , I you can never
46:05
underestimate how powerful that is but
46:07
also the possibilities that there's millions
46:10
of people out there that need to hear about this , that
46:12
are suffering , and some of them I think
46:14
some of them are having early mortality . Some
46:16
of them are dying as a result
46:18
of this lack of knowledge .
46:19
Suffering silently because they've never
46:22
actually known about it .
46:24
Right , and it's
46:26
exciting because the needle is starting to move a little
46:28
bit . We just recently got one of the medications
46:31
for specifically for vulnerable brains which talked
46:33
a lot about , just got an indication
46:35
for preventative treatment . That's not been something
46:37
that's really been on the market and so
46:39
that's exciting . There's some movement there . We know that
46:42
there's some new studies coming out , new therapies
46:44
coming out down the line . It is really
46:46
exciting to think what could be solutions in
46:48
the future . But I certainly hope anybody
46:50
listening to this podcast today I hope you've been inspired
46:52
and energized and excited about the
46:54
possibilities and what
46:57
you could learn and I know we're
46:59
preaching to the choir here because if you're listening to this , you
47:01
obviously are already self-learning , which
47:03
is great , but we want you to get involved
47:05
. We're real people with an office that we take
47:07
calls every day , all day , and we want to make certain
47:09
that people can call us and just reach out
47:11
, pick up the phone . I mean , you know , if you
47:13
just call the main 800 number , you're going to get somebody
47:15
that's a caring , thoughtful
47:20
person that's going to want to hear your story out and listen , and we might
47:22
very well have some tools that we can send you or empower you with that can help you
47:24
to have some of those important conversations and
47:27
so hard of hope , yeah , so
47:29
true . So , biven , thank you so much
47:31
for for being
47:34
invested , because I know every minute
47:36
that you spend away from family and your
47:38
career and everything else I know is a sacrifice
47:41
, and and and I just want to say
47:43
thank you so much for being invested with us as a
47:45
board member to help guide us down this journey
47:47
, to learn how to , how to explore and expand
47:49
our reach , but also thank you for
47:51
taking the time today to just invest in
47:53
this moment my pleasure . Thanks for having me . Well
47:56
, thank you so much for listening to this podcast . I hope
47:58
it was encouraging to you . You can find more resources
48:01
on hope-charitiesorg
48:03
and we would love , love , love for you
48:05
to get involved in one of those events we talked about . But
48:08
also , we're really excited about the future
48:10
of what we can do together , and so we need you
48:12
to get invested with what
48:14
we're doing here , because there's so much more to
48:17
do and we can only do it with your help . So , thanks so much for
48:19
listening to this podcast . We hope to see you on
48:21
the next one . Take care .
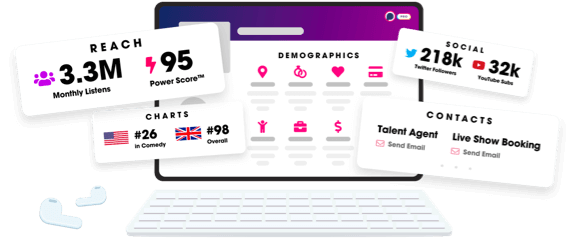
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
