This podcast “Apalutamide in Metastatic Castration-Sensitive Prostate Cancer (mCSPC): A Case-Based Discussion” was originally presented as an AUA newsworthy webinar and contains data regarding the clinical efficacy and safety of apalutamide. It is presented on behalf of Janssen and is not certified for CME; speakers were compensated. For full details, see the video webinar here.
TITAN, a Phase 3 double-blind study, randomized patients with metastatic castration-sensitive prostate cancer (mCSPC) to apalutamide (Apa; 240 mg oral once daily) + androgen deprivation therapy (ADT; n=525) or placebo + ADT (n=527).1,2 All patients received a concomitant gonadotropin-releasing hormone analog or had prior bilateral orchiectomy.3 Patients who received prior treatment for localized disease or received but did not progress on docetaxel were permitted. Dual primary endpoints were radiographic progression-free survival and overall survival (OS).1,2
At primary analysis (median follow-up: 22.7 months), Apa + ADT reduced the risk of radiographic progression or death by 52% vs placebo + ADT (HR: 0.48; 95% CI: 0.39–0.60). Apa + ADT also reduced the risk of death by 33% vs placebo + ADT (HR: 0.67; 95% CI: 0.51–0.89).1 At primary analysis cutoff, TITAN was unblinded and 39.5% of patients who received placebo + ADT crossed over to receive Apa + ADT; these patients were analyzed as part of the placebo + ADT population in the intent-to-treat analyses. The IPCW log-rank test was performed to account for crossover and showed a 48% reduction in the risk of death for Apa + ADT vs placebo + ADT (HR: 0.52; 95% CI: 0.42–0.64). At final analysis (median follow-up: 44.0 months), Apa + ADT reduced the risk of death by 35% vs placebo + ADT (median OS: NE vs 52.2 months; HR: 0.65; 95% CI: 0.53–0.79).
In a prespecified subgroup analysis, Apa + ADT improved OS vs placebo + ADT, regardless of disease volume. In patients with high-volume disease, Apa + ADT reduced the risk of death by 30% vs placebo + ADT (HR: 0.70; 95% CI: 0.56–0.88); for low-volume disease, Apa + ADT reduced the risk of death by 48% vs placebo + ADT (HR: 0.52; 95% CI: 0.35–0.79).2
The following post hoc analyses data are not included in the full ERLEADA® (apalutamide) Prescribing Information.
Post hoc exploratory analyses investigated PSA kinetics.4,5 After 3 months of Apa treatment, median OS was not reached in patients with a PSA response. In patients without a PSA response, median OS was 37.7 months.5 Most Apa + ADT-treated patients had undetectable PSA at 3 months. By 12 months, 64% of Apa-treated patients had undetectable PSA vs 23% of patients treated with placebo + ADT.5
Please see the full Prescribing Information for ERLEADA® (apalutamide) at www.erleadahcp.com.
- Chi KN, et al. N Engl J Med. 2019;381:13–24.
- Chi KN, et al. J Clin Oncol. 2021;39:2294–2303.
- ERLEADA® (apalutamide) [Prescribing Information]. Horsham, PA: Janssen Biotech, Inc.
- Chowdhury S, et al. Ann Oncol. 2023;34:477–485.
- Chi KN, et al. Presented at AUA; September 10–13, 2021; Las Vegas, Nevada.
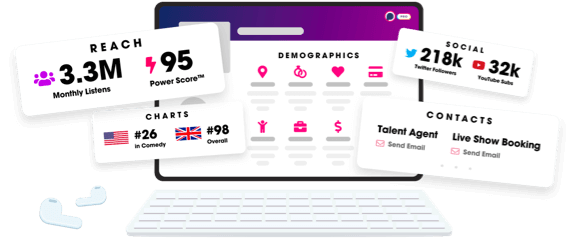
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
